Diet
Histamine is produced by mast cells in the body. However, it is also found in many foods and is ingested with them and stored in the body. Some foods are rich in histamine by nature, in others they develop in a process of fermentation. Histamine is present in great quantities in spoiled food and can cause symptoms of food poisoning even in healthy persons (e.g. the so-called “fish poisoning”).
Normally histamine ingested with food is degraded in the small bowel by diamine oxidase (a special enzyme). However, if there is a deficiency of this enzyme or if large quantities of histamine have been ingested, the existing diamine oxidase is insufficient to degrade the histamine quickly, and passes from the mucous membrane of the small bowel into the blood. The body then reacts with symptoms such as urticaria, an urge to sneeze, headaches, asthma and/or diarrhoea. Allergy tests are not of help as this is not a case of food allergy.
How can a low-histamine diet work for me with my urticaria?
Patients often report that their urticaria worsens after eating food with high amounts of histamines. Studies have shown that a diet, in which food with high amounts of histamine are abstained from can lead to a clear improvement or even cure of urticaria.
What food should I avoid?
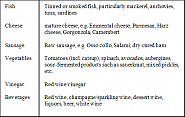
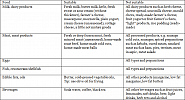
In a low histamine diet smoked, salted, fermented, baldy stored or marinated foods are strictly banned. The following foods should be completely abstained from during a low-histamine diet as they contain large amounts of histamine (Ill. 1).
By the interaction with other food factors the effect or quantity of the histamine ingested may be increased. Particularly alcoholic beverages, coffee and black tea, bear a hazard. Furthermore, the degradation of histamine may be inhibited by various drugs. In as far as possible these drugs should be avoided or, if necessary and in consultation with your doctor, switched to another active ingredient (Ill. 2).
How can I subsist on low-histamines and yet enjoy a varied and high-value diet?
In general: Wherever possible use fresh, unprocessed foods. To assist you in your choice please turn to the following food list in which the food you can eat and drink without hesitation is listed.
Dairy products
- whole milk, pasteurised
- skimmed milk and UHT milk
- sweet and sour cream
- sour milk*
- butter milk*
- farmer’s cheese*
- cream cheese*
*Do not store these products for a long time
Meat
- not matured beef*
- veal
- pork
- lamb
- poultry
- ham - cooked
- eggs
*frozen directly after slaughter
Fish
- Fish products*
- plaice
- cod
- shellfish
- perch – ocean perch
- pollock
- hake
- trout
*Freshly caught fish or quickly frozen.
Fish bedded on ice cubes, may, according to the law, be up to 1 week old and thus rather unsuitable.
Bread spreads
- butter
- margarine
- honey
- home-made jam*
* Important: process fresh fruit immediately
Confectionery
- fruit drops
- fruit gums
- sherbert sweets
- chewing gum
- popcorn
Dessert
- vanilla pudding or
- Dessert powder for cold mixing
- fruit soups*
- fruit farmer’s cheese*
- stewed fruit*
- fruit or cream ice cream*
- rice pudding*
* best home-made with suitable fruit
Fruit
- all fresh and deep frozen fruit
Vegetable
- all fresh and deep frozen vegetables except: Tomatoes, avocados,spinach, aubergines
Cereal products
- Grains/seed
- Tubers
- Bread and pastry
- Cereal flakes
- Pasta
- Fresh or dried cereal grains and others (maize, millet, rice buckwheat) except sprouts
- all types of potatoes
Beverage
- Soda water
- home-made fruit and Vegetable juice
What is a pseudoallergy?
Pseudo-allergies (fake allergies) are intolerance reactions of the body characterised by symptoms such as found in allergy patients, they may manifest themselves e.g. with wheals and angioedema, breathing or swallowing disorders or diarrhoea.
Unlike in the case of a “true” allergy, pseudoallergies are not based on inducing antibodies. (“defending proteins”) and depend on dose, i.e. the more a particular substance is ingested, the severer the symptoms. Food additives such as colorants and preservatives, drugs, but also substances natural in foods such as flavourings are frequent triggers of pseudoallergy.
How do I know that my urticaria is caused by a pseudoallergy?
Pseudoallergy cannot, as in a classical allergy, be determined by a simple blood or skin test. Only a diet can lead to the correct diagnosis. If urticaria improves in the course of the diet, urticaria is probably caused by pseudoallergic reactions to certain food additives. If urticaria worsens after provocation with pseudoallergy rich food, it is surely a case of pseudoallergy. If pseudoallergy is suspected, a low-pseudo-allergen diet should be kept.
May I never eat food with additives again?
Frequently patients suffering from a pseudoallergy can completely stop keeping a low-pseudo-allergen diet after 6 to 18 months. The reason is still unclear. Possibly the intestinal mucosa change in the course of the diet which results in the intestines no longer being able to absorb the pseudo-allergens so easily. The body then “forgets” to trigger itchiness and wheals.
During the first four weeks all foods rich in pseudo-allergen should be abstained from (s. table). Exclusively such foods as in the “suitable” column should be ingested. As from the 5th week one of the foodstuffs listed in the not suitable” column may be tested. This foodstuff should be eaten several times a day on 3 subsequent test days. If no symptoms are triggered, this foodstuff may be eaten from now on and a new foodstuff can also be tested immediately.
If symptoms increase during the test days, the tested food should no longer be ingested and avoided in future. After some time patients know their own individual, compatible diet and possibly only have to abstain from a few foodstuffs. When on the diet and the following restorative phase antihistamines are only administered when needed to be able to appraise a possible deterioration.
How do I keep on track?
In order to keep track on which foodstuffs have already been tested and what the reaction was, a diary should be kept on the food eaten should be noted. You mark all the foods of the “not suitable column” and which you tested clearly in another colour. If you have tolerated the food after 3 test days, it changes over to the “suitable column” and you no longer have to avoid it.
Dietary mistake – What should I do?
Food rich in pseudo-allergen can often not be avoided, particularly when eating out. If a dietary mistake occurs as exception, it is not all over. You most probably won’t see a change of your skin. The reason is that a pseudoallergy depends on the dose, i.e. the more food rich in pseudo-allergen you eat, the worse your skin gets.
Choice of food in low pseudo-allergen food
In general the following applies: Use fresh and unprocessed food! The following terms indicate the presence of additives: E100–E1518, colorant, preservation substance, gelling agent, thickening agent, humectants, emulsifier, taste enhancer, antioxidant, separating agent, glazing agent, sweetener, raising agent, glazing agent, firming agent, flour treatment agent, modified starch, foaming agent, anti-foaming agent, molten salt, stabiliser, flavouring (agents).
However: The following foods may contain additives without them being indicated:
- unpacked, processed food (e.g. bread, cake, biscuits, sausage, delicatessen salads)
- potato products (croquettes, French fries, pre-peeled potatoes etc.)
- many alcoholic beverages, chocolate, filled chocolates, foods of compound ingredients (e.g. fruit preparations in yogurt)
We have compiled a list with foods suitable, or not suitable for a pseudo-allergen-free diet. 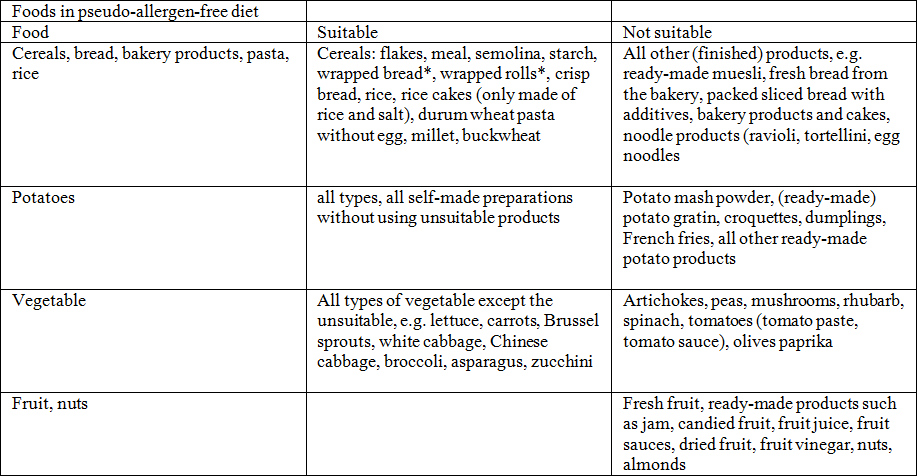
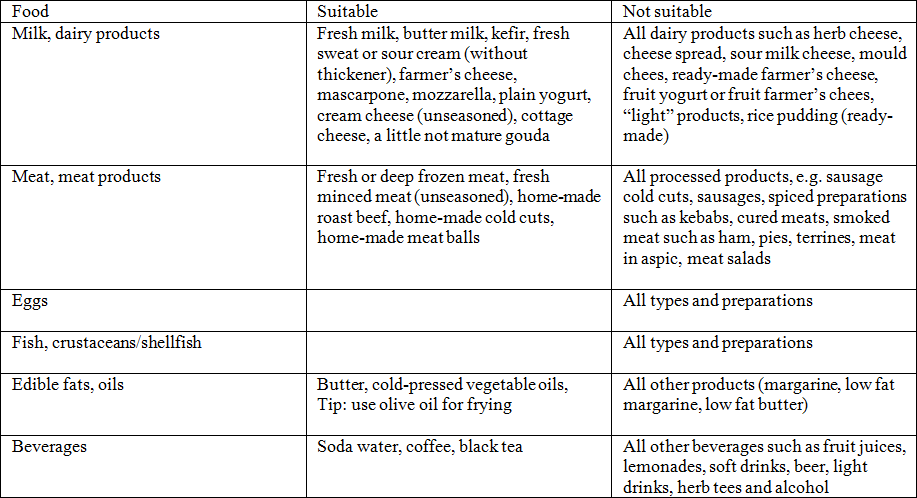
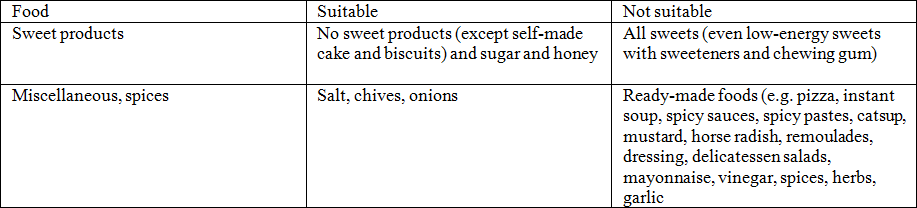
There is no claim on this list being exhaustive (mod. Acc. T. Zuberbier, B.M. Czarnetzki., Food intolerances (II). Dermatologist 1993; 44: 57–62, provided by I. Ehlers, Charité Berlin).



 English
English Deutsch
Deutsch Francais
Francais Español
Español